World Leprosy Day
The last Sunday of January each year is observed as World Leprosy Day (January 25, 2026). This day aims to raise public awareness of leprosy (also known as Hansen's disease), eliminate discrimination and prejudice against affected individuals, promote early diagnosis and treatment, and advance the global goals of "zero transmission, zero disability, and zero discrimination."
1 Disease Overview and Global Burden of Leprosy
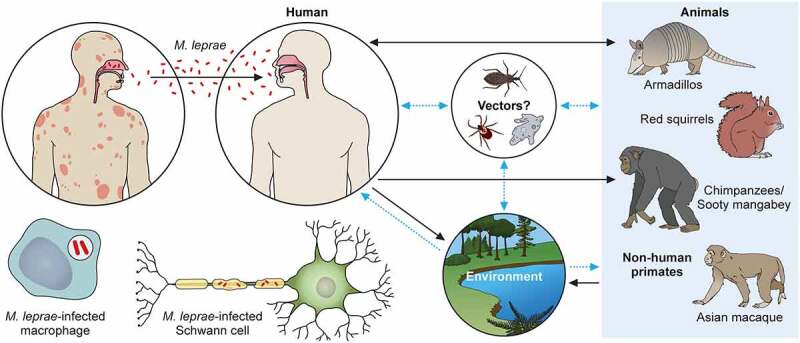
Leprosy is a chronic infectious disease caused by Mycobacterium leprae, which primarily affects the skin, peripheral nerves, upper respiratory mucosa, and eyes. The bacterium grows extremely slowly and has a long incubation period; some patients may develop clinical symptoms only years or even decades after infection, posing significant challenges for early detection and intervention. According to the World Health Organization (WHO), approximately 200,000 new cases are still reported globally each year, mainly in certain developing countries and tropical regions, indicating that leprosy remains a public health concern that cannot be ignored.

Leprosy itself is not highly fatal, but without early diagnosis and timely treatment, persistent immune-mediated inflammation can lead to severe peripheral nerve damage, resulting in sensory loss, muscle atrophy, limb deformities, and vision impairment. These irreversible complications are the primary causes of disability and social marginalization among patients and represent a core challenge in leprosy control efforts.
2 Immunological Mechanisms of Leprosy
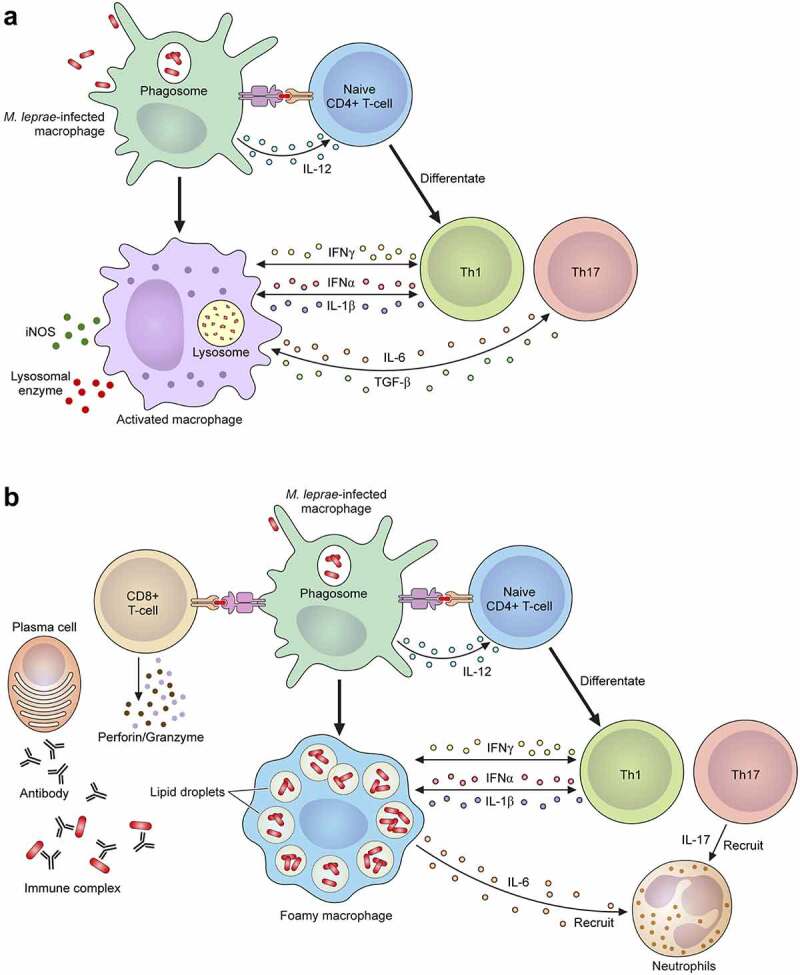
In terms of pathogenesis, leprosy is a classic example of an infectious disease whose outcome is determined by the host immune response. Immune responses to Mycobacterium leprae vary significantly among patients, forming a continuous disease spectrum ranging from tuberculoid leprosy to lepromatous leprosy. Patients with a dominant Th1 cell-mediated cellular immune response can better restrict bacterial replication, presenting with relatively localized clinical manifestations. In contrast, patients with a Th2-biased humoral immune response often develop high bacterial loads, widespread skin lesions, and severe nerve damage.
During disease progression, macrophages, Schwann cells, T-cell subsets, and various inflammatory cytokines and chemokines are involved in the pathological process. Particularly during leprosy reactions (such as Type 1 and Type 2 reactions), excessive or imbalanced immune activation is a key mechanism leading to acute nerve injury and tissue destruction. Therefore, a deeper understanding of the immune pathways and molecular markers associated with leprosy is crucial for early diagnosis, disease classification, and the development of new intervention strategies.
The WHO primarily classifies leprosy into paucibacillary and multibacillary types, which is essential for determining treatment regimens. However, from an immunopathological perspective, the traditional five-type classification based on clinical, bacteriological, and immunological features is more commonly used, with "tuberculoid" and "lepromatous" representing the two extremes of the immune response spectrum.
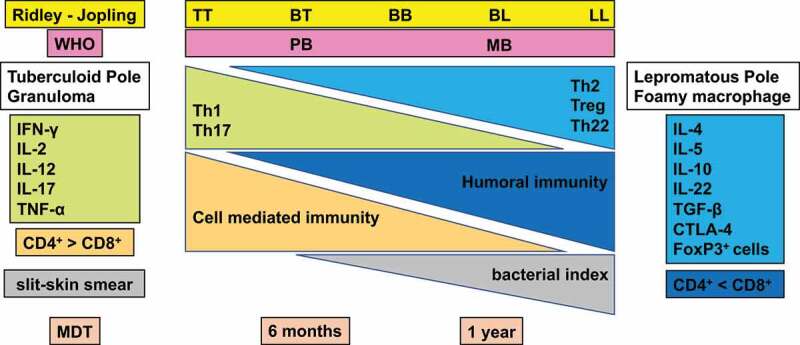
2.1 Tuberculoid Leprosy
Tuberculoid leprosy lies at one end of the disease spectrum, characterized by a strong cellular immune response to M. leprae. This results in localized lesions, typically presenting as few, well-defined hypopigmented or erythematous plaques, often accompanied by significant sensory reduction or loss. Bacterial load in the lesions is very low or undetectable, making this form less contagious. The pathological hallmark is a granulomatous inflammatory response with dense lymphocyte infiltration around nerves. While this effectively restricts bacterial spread, it is also a major cause of nerve damage and dysfunction. Therefore, even after the disease is controlled, managing long-term neurological sequelae remains a key focus of rehabilitation.
2.2 Lepromatous Leprosy
Lepromatous leprosy lies at the opposite end of the spectrum, where patients have a severely deficient or absent cellular immune response to M. leprae. This leads to systemic, disseminated infection with widespread, symmetrical, infiltrative nodules, plaques, and papules on the skin. Facial involvement can result in the characteristic "leonine facies." Mucous membranes, lymph nodes, and visceral organs may also be affected. Lesion tissues contain large numbers of M. leprae bacilli, making this form highly contagious. The pathological feature is the accumulation of lipid-laden foamy macrophages (lepra cells), forming typical globi. Due to the lack of effective immune containment, disease progression is more insidious and extensive. Nerve damage, although occurring later, is equally severe and tends to be symmetrically distributed.
Between tuberculoid and lepromatous poles, there exist borderline tuberculoid, mid-borderline, and borderline lepromatous forms, completing the full immunological spectrum of the disease. This classification not only reflects disease severity and infectiousness but also profoundly influences treatment strategies and prognosis.
3 Current Status and Challenges in Diagnosis and Treatment
Treatment for leprosy has evolved from single antibiotics to multidrug therapy (MDT), recommended by WHO and consisting of rifampicin, dapsone, and clofazimine. MDT effectively kills M. leprae, reduces treatment duration to 6-12 months, and significantly lowers relapse rates. However, repairing nerve damage remains a major challenge. Recent research focuses on neuroprotective strategies, such as the application of neurotrophic factors (e.g., NGF), stem cell transplantation techniques, and immunomodulators (e.g., IL-10 inhibitors), to promote nerve regeneration and functional recovery. Additionally, molecular diagnostic techniques (e.g., PCR for detecting M. leprae DNA) are being implemented at the primary care level to improve early screening sensitivity. Vaccine development (e.g., candidate vaccines based on M. leprae proteins) is also entering clinical trial stages, offering potential prevention for high-risk populations.
4 AntibodySystem Supports Leprosy Mechanism Research
On World Leprosy Day, focusing not only on the disease itself but also on scientific research and technological advances is a vital force in driving the eventual elimination of leprosy. AntibodySystem remains committed to supporting global researchers in the field of leprosy and related immune diseases with high-quality products.
| Catalog | Product Name |
|---|---|
| YXX21301 | Recombinant Mycobacterium leprae Secretion protein EspA Protein, N-His-KSI |
| PXX21301 | Anti-Mycobacterium leprae Secretion protein EspA Polyclonal Antibody |
